Over the course of a decade, I met Dad’s care with grace, honor and his infectious sense of humor. Celebrating, his living and loving was the Leiner-way. He’s been gone for two months and my heart and car are still on auto-pilot. In that blissful split second I think I will visit, I forget and then remember. There is joy-tinged grief in letting the “before” memories flood back into focus. It has felt as if I have lost two guys. I am realizing how I kept the dad before memory loss at bay to be able to meet him in the moment. Yes, even as a grief specialist, with all of the tools and training, nothing feels right, right now.
Dad was a retired “Mad Man”, with nearly three decades at the same ad agency. He worked on breakthrough pharmaceutical launches with top docs around the world. His brilliant brain faded from Alzheimer’s before our eyes, as the research raged on.
When he forgot the very familiar route from my sister’s house, we knew it was time for an intervention. The neurologist who diagnosed his MCI (mild cognitive impairment) never shared any parting advice about best practices, dietary changes, Dad’s safety or even a book or website with us. There was certainly not a whiff, word or single hint about what caretaking might look like for my single Dad and three siblings.
We learned to live through each change, navigating the delicate balance of our own households and his growing needs. Each time we averted a crisis, (and there were many) I felt the need to shout our learnings from the proverbial rooftop. “Quick, tell the others!” Books and websites are helpful, but there was much that felt particular to us, our family and his ever-changing needs.
CALL FOR HELP:
I wish we had known this sooner. First, we cobbled together a family team. Then we brought in someone who helped him tidy and asked if she would check in a few hours a day. Dad was prescribed a patch that was meant to slow the disease. It needed to be placed out of his reach and changed every 24 hours. He affectionately called them, “The Patchers”. Finding help is not easy and quite costly. Explore what insurance may cover, if there are local programs for daycare and even meal services.
NEW SYSTEMS:
When his cell was left unanswered and the landline was our only connection, we swapped it for a photo phone. We programmed big buttons with our pics to autodial. We put outfits in a basket, so he knew what to wear each day. These work, until they don’t and you find another way.
WISHES & MEDICAL ORDERS:
He wanted to stay in his home, until he could not. While his memory was still sharp-ish, we had hard conversations. “The simplest pine box, please. Nothing fancy,” he said. He gave us permissions and passwords. We talked about his will and finances. We put a limit on the amount of cash he took from the bank for pocket money. Preserving his autonomy and dignity were non-negotiables.
We named a power of attorney and healthcare proxy. In New York, a MOLST (Medical Orders for Life Sustaining Treatment) is co-created with a physician. This hot pink paperwork and meds list traveled with him everywhere. We updated it often and kept copies on all of our phones. Find out what works in your state. Shockingly, he was sent by ambulette alone, many times, arriving at the hospital before family.
THE MOVE:
We moved Dad to an assisted living apartment and made it as warm and familiar as possible with his art, furniture and piano. We brought the party to Dad. From Fudgey The Whale birthdays to bagel bash holidays his life was a celebration, replete with balloons, Ray Charles playlists, grandkids and grand dogs. We read to him, created photo albums and enjoyed picture books and stories.
WIPE BOARDS:
The wipe board in his home and hospital room were headquarters for the shorthand we wanted him and others to know. I have dementia. I am hard of hearing and wear hearing aids. Call me Neil.
HOSPITAL STAYS:
The staff are not trained or savvy in caring for memory loss or elders. We took turns spending the night and communicated on his behalf. Everything from meal orders to advocating for his level of care and comfort were on us. Someone living close, or a plan of action is helpful.
PALLIATIVE CARE & HOSPICE
Become familiar with healthcare services that are aimed at optimizing quality of life and reducing suffering. This is life giving, especially with a terminal illness. They take care of caretakers too.
Finally, please care of you too! Find breaks and laughter. Befriend the anticipatory grief you’ll meet along the way. Most of all, love what is left. There is so much beauty and peace in looking back as I look forward. Folks remarked, “he must have been a great Dad” in witnessing his care. Caring for him alongside my sibs was the honor of my lifetime.
There is a free Grief Relief Kit on my site along with my favorite resources, books, and podcasts, stop on by and pick it up! Or book a complimentary consultation. I am here for you. x, Barri
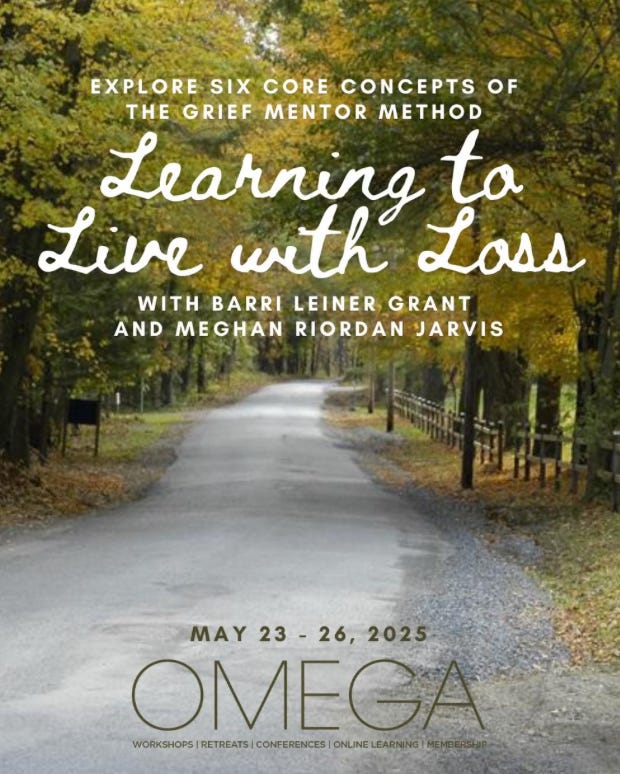
Meet me in May at Omega. Learn more here.














Share this post